In December 2019, a novel coronavirus COVID-19 was found to produce clusters of acute respiratory illness in Wuhan, China, now known as novel coronavirus–infected pneumonia (NCIP).
Deaths due to COVID-19 infection primarily occur in patients transferred to the ICU with NCIP. These patients have or develop severe respiratory distress and full blown ARDS. In such cases, treatment requires mechanical ventilation for respiratory failure.
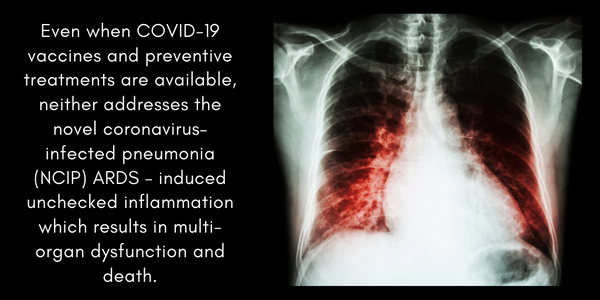
However, patients with NCIP-induced ARDS often succumb to multi-organ failure. There are two threats. First, organ failure that occurs is a direct result of unremitting inflammation generated by the virus-activated innate immunity pathways designed to contain the viral infection. A second and very important threat is where inflammatory pathways are activated by exposure to mechanical ventilation.
Activation of these evolutionarily-conserved inflammatory pathways results in massive increases in the circulating levels of inflammatory cytokines which produce vascular leak, edema of multiple critical organs (lung, kidneys, heart, brain, liver, GI tract) and ultimately result in multi-organ dysfunction and death. These abnormalities were previously observed in patients who did not survive MERS-CoV and SARS-CoV infection. The overall inflammatory burden produced by the virus and by the ventilator drives the occurrence of severe, and often fatal organ failure.
While COVID-19 vaccines and anti- COVID-19 drugs are of obvious utility, availability of these therapies is not imminent. Even when these treatments were to become available, neither therapeutic strategy addresses the pathobiology of NCIP-ARDS-induced unchecked inflammation which results in multi-organ dysfunction and death. Without the availability of FDA–approved ARDS therapies, specific treatments do not exist for coronavirus infection except for supportive care and meticulous precautions to reduce viral transmission. Antibacterial agents, antiviral agents and methylprednisolone have been shown to be ineffective in viral-induced ARDS and were ineffective in treating severe SARS and MERS. Early reports indicate that antibacterial agents, antiviral agents and methylprednisolone are ineffective in NCIP-induced ARDS. Furthermore, while SARS and MERS were self limited outbreaks with high case fatality, and the current COVID-19 pandemic with a case fatality rate of 2% is also likely to eventually run its course, ARDS resulting from sepsis, trauma and a myriad of diverse stimuli will continue to be an ongoing unmet therapeutic need.
The Aqualung Therapeutics Solution
ARDS is the lead clinical indication for Aqualung Therapeutics and extracellular nicotinamide phosphoribosyltransferase (eNAMPT) and its receptor, Toll-like receptor 4 (TLR4), have been identified by Aqualung scientists as a key targetable upstream inflammatory cascade that contributes to ARDS morbidity and mortality. Aqualung Therapeutics has developed eNamptorTM, a Next Gen platform comprised of: i) ALT-100, a humanized eNAMPT-neutralizing monoclonal antibody, ii) eNAMPT-Plex, a plasma-based biomarker panel comprised of cytokines, including eNAMPT, which predicts ARDS mortality; and iii) NAMPT-Gene, a genotyping assay that identifies individuals with NAMPT genetic variants at increased risk for ARDS death. Supported by strong preclinical and human data, combining the elements of the eNamptorTM platform technology has the potential to define high risk ARDS individuals as well as identify patients most likely to respond to ALT-100 and reduce downstream inflammation that contributes to death from NCIP and NCIP-ARDS.